What are bed sores ?
What are bed sores?
The injuries or ulcers that happen on the skin or underlying tissues due to the prolonged pressure on the skin are called as the bed sores. Bedsores are ulcers that happen on areas of the skin that are under pressure from lying in bed, sitting in a wheelchair, or wearing a cast for a prolonged time.
They are also called as the Pressure Ulcers/Pressure Sores as they can form due to the prolonged pressure on the skin. The friction, moisture, immobility are some major causes of bed sores. It can harm your inner skin or even the bones in the severe conditions.
Photos of Bed Sores


Bed Sores Symptoms:
- Redness of the skin.
- The area with bed sore may feel warmer and painful than the other body parts.
- Infection can observed.
- Pus like draining can be seen. I
- f the ulcer is deep, the skin can be seen broken.
Causes of Bed Sore:
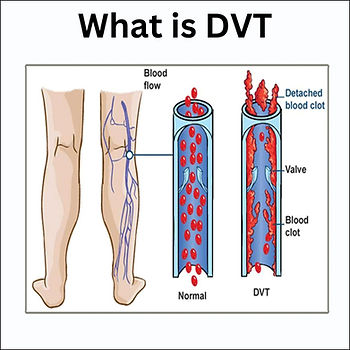
- Pressure: In a person the blood Flow can get lessen due to the immobility. Blood is the connective tissue which supplies Oxygen and Nutrients to all parts of the body. The pressure risen due to the immobility of a person can reduce the blood flow at the site of the contact of body and the surface. This leads to the formation of Bed Sores.
- Friction: When a body surface gets rubbed against the bed or the surface laid below the friction can be seen generated. Friction leads damaging of the upper portion of the skin.
- Moisture: The moist skin is a major cause for the friction.
- Age factor: The blood flow can get lessen due to the age of a person which may result in the forming of the bed sores.
- Obesity
- Immobility: Immobility of a person can cause the reduction of the blood flow and increase in the pressure and friction which can cause the be sores.
- Poor nutrition
Common sites for Pressure Ulcers
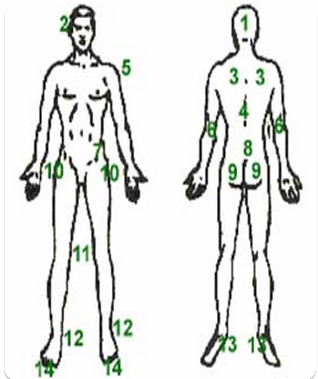
- Occiput/ Back of Head
- Ears
- Scapula
- Spinous Process
- Shoulder
- Elbow
- Iliac Crest
- Sacrum/Coccyx
- Ischial Tuberosity
- Greater Trochanter
- Knee
- Malleolus
- Heel
- Toes
How to Prevent The Risk?
- Keep the older patients moving
- Position immobile/dependent patients frequently and carefully
- Keep incontinent patients clean and dry
- Assist with meals and snacks
- Maintain adequate hydration
- Be alert to changes in skin and report them
- Consider the impact of medical equipment in use. It may cause pressure ulcers
- Manage and support the patient’s pain effectively
- Reduce overheating
- Re-assess risk factors regularly
- Use Air Mattresses
References:- 1) Mayoclinic Website
2) Johns Hopkins Website